Introduction
The relationship between your gut and heart is much deeper than most realize. Recent science shows that the gut microbiome — the vast community of bacteria living in your digestive tract — plays a central role in maintaining heart health and achieving an optimal heart. Factors like TMAO, fiber intake, fermented foods, and probiotics can all influence cholesterol, inflammation, and overall cardiovascular outcomes. Understanding these interactions empowers individuals to make food choices and lifestyle changes that support both gut and heart health. This article explores the key mechanisms and practical strategies that link the microbiome to your heart’s wellbeing.
What is the Gut‑Heart Axis?
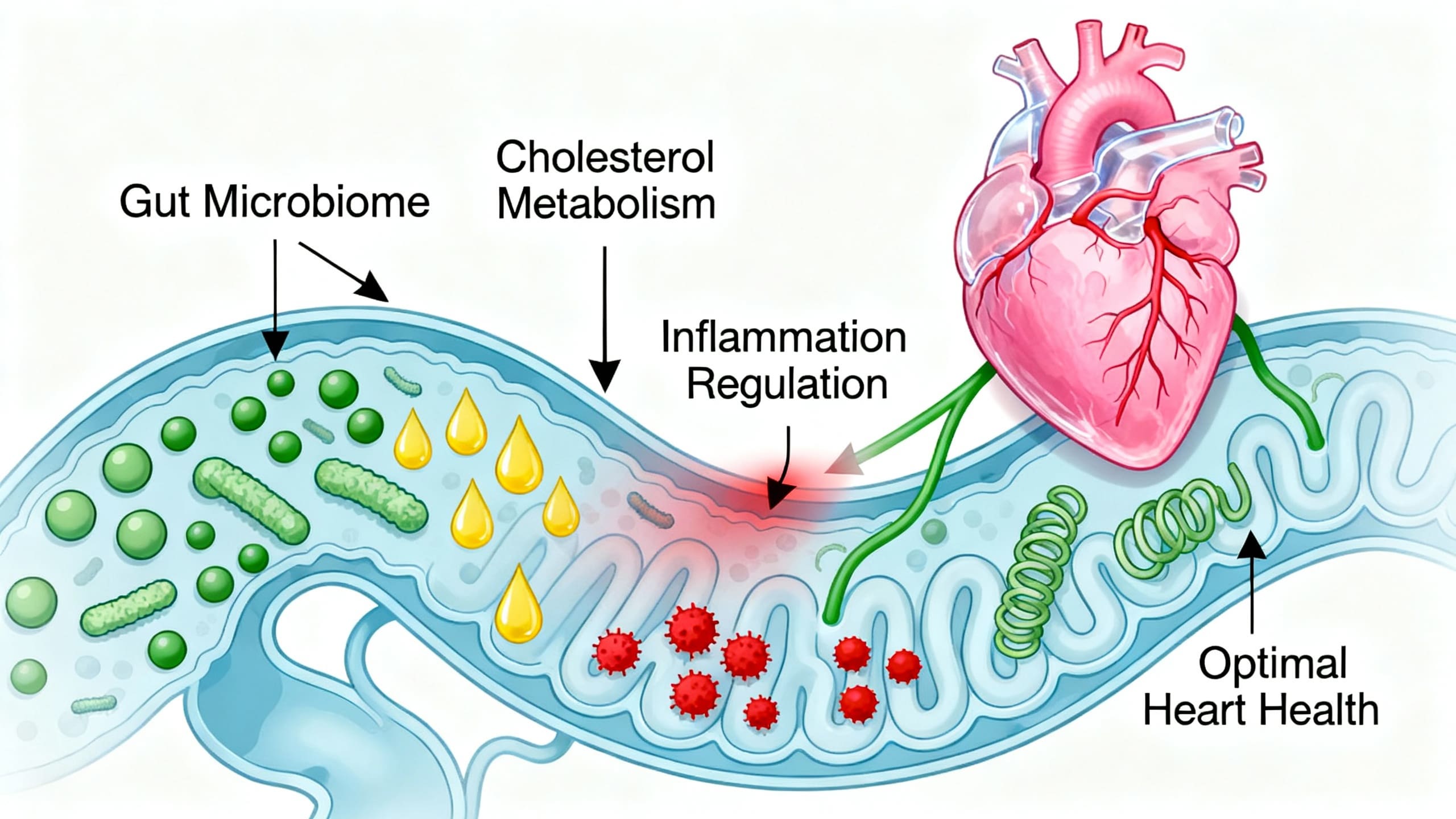
The gut-heart axis refers to the dynamic, two-way communication between the gut microbiome and the cardiovascular system. Researchers have discovered that the byproducts of gut bacteria, especially TMAO (trimethylamine N-oxide), and nutrients like fiber, significantly affect vascular health and inflammation levels (Jonsson & Bäckhed, 2017). The concept originated from studies showing that gut microbes can produce molecules that directly impact heart function and disease risk (Witkowski et al., 2020). Maintaining a healthy, diverse gut microbiome is increasingly recognized as a foundation for optimal heart outcomes.
Benefits and Outcomes in Heart Disease
A balanced gut microbiome can influence heart health in several scientifically supported ways:
- TMAO Reduction: Certain gut bacteria convert dietary choline and carnitine to TMAO, a compound linked with higher plaque formation and heart disease risk (Koeth et al., 2013). Foods high in fiber and probiotics help decrease TMAO levels.
- Lower Blood Pressure: Fiber fermentation produces short-chain fatty acids (SCFAs), which reduce inflammation and help lower blood pressure (Morrison & Preston, 2016).
- Cholesterol Management: Probiotics and fermented foods assist in breaking down cholesterol, limiting its absorption and supporting optimal heart function (Kumar et al., 2022).
- Reduced Inflammation: High-fiber diets and regular intake of fermented foods are associated with lower levels of CRP, a key inflammatory marker in heart disease (Tang et al., 2019).
- Anti-Clotting Effects: Certain beneficial bacteria may reduce the formation of harmful clots by balancing platelet activity (Witkowski et al., 2020).
Research Insights
Landmark human studies and systematic reviews provide robust insights into the gut-heart axis:
- A major clinical trial found elevated TMAO linked to higher heart attack risk, independent of other factors (Koeth et al., 2013).
- Randomized controlled trials show high soluble fiber diets can reduce LDL cholesterol and blood pressure, markers crucial for heart health (Morrison & Preston, 2016).
- Systematic reviews confirm that probiotic supplements, especially strains like Lactobacillus and Bifidobacterium, modestly lower cholesterol and inflammation (Kumar et al., 2022).
- Consensus guidelines recommend fermented foods and prebiotic fibers for general heart health benefits (Tang et al., 2019).
Practical Applications
Understanding the gut-heart axis allows for practical steps toward maintaining heart health and achieving an optimal heart:
- Meal Ideas: Incorporate high-fiber foods (oats, legumes, berries), probiotic-rich foods (yogurt, kefir, kimchi), and prebiotic foods (onion, garlic, asparagus) into daily meals (Morrison & Preston, 2016).
- Safe Supplementation: Probiotics are generally safe for healthy adults at doses up to 10–20 billion CFUs per day (Kumar et al., 2022). Always choose reputable brands and consult a doctor for specific health conditions.
- Who Benefits Most: Individuals at risk for or with early-stage cardiovascular disease, those with high cholesterol, or those eating a low-fiber diet stand to gain the greatest benefits from these interventions (Jonsson & Bäckhed, 2017).
- Fermented Foods: Adding at least one serving of fermented foods daily, such as sauerkraut or miso, can support a healthy gut microbiome.
Risks & Limitations
While evidence is strong, some limitations remain:
- Individual Variability: The exact effect of microbiome interventions can vary widely among individuals (Witkowski et al., 2020).
- Probiotic Safety: Immunocompromised individuals should avoid certain probiotics due to infection risk (Kumar et al., 2022).
- Research Gaps: More large-scale, long-term clinical trials are needed to determine the best mix of foods and bacteria for heart health (Jonsson & Bäckhed, 2017).
- Not a Standalone Solution: These approaches work best alongside conventional heart health measures, such as medication and regular exercise.
Key Takeaways
- The gut microbiome critically influences heart health through compounds like TMAO and fiber fermentation.
- High-fiber and fermented foods, along with probiotics, are proven strategies for an optimal heart.
- Modifying the gut-heart axis can reduce cholesterol, blood pressure, and inflammation.
- Clinical support for using these interventions is strongest for those at higher cardiovascular risk.
Frequently Asked Questions
Q1: Can eating more fiber really help my heart health?
Yes. High-fiber diets are linked with reduced cholesterol and lower heart disease risk by influencing gut microbiome activity (Morrison & Preston, 2016).
Q2: What is TMAO and why is it important for heart health?
TMAO is a gut bacteria byproduct tied to higher atherosclerosis and heart disease risk (Koeth et al., 2013). Lowering TMAO helps achieve an optimal heart.
Q3: Are all probiotics helpful for cardiovascular health?
Not all probiotic strains have cardiovascular benefits. The best evidence supports Lactobacillus and Bifidobacterium for cholesterol and inflammation management (Kumar et al., 2022).
Q4: Is it safe to take probiotic supplements daily?
For most healthy adults, yes; probiotics are safe up to 10–20 billion CFUs per day. Immunocompromised people should consult their doctor (Kumar et al., 2022).
Suggested Links
- American Heart Association – Healthy Eating & Gut Microbiome
- NIH – The Human Microbiome Project
- PubMed – Gut Microbiome and Cardiovascular Disease
Conclusion
The gut-heart axis is a game-changer for understanding and achieving optimal heart health. By embracing meals rich in fiber, fermented foods, and science-backed probiotics, we can favorably influence cholesterol, inflammation, and our risk of heart disease. Consistently prioritizing gut health is a practical and powerful step toward lifelong cardiovascular wellness. For best results, combine these dietary shifts with guidance from a healthcare professional and proven heart-healthy practices.