Introduction
Intermittent fasting—encompassing strategies like time-restricted eating and alternate-day fasting—has rapidly gained popularity among those seeking better heart health, improved metabolic flexibility, and overall wellness. These dietary approaches have been highlighted for their potential to lower triglycerides, enhance insulin sensitivity, and contribute to an optimal heart. As cardiovascular disease remains the leading cause of death worldwide, understanding how these fasting techniques relate to heart health is crucial. This article delves into the evidence behind intermittent fasting, its practical impact on heart disease prevention, and tips for maximizing heart health outcomes.
What is Time-restricted Eating, Alternate-day Fasting, and Metabolic Flexibility?
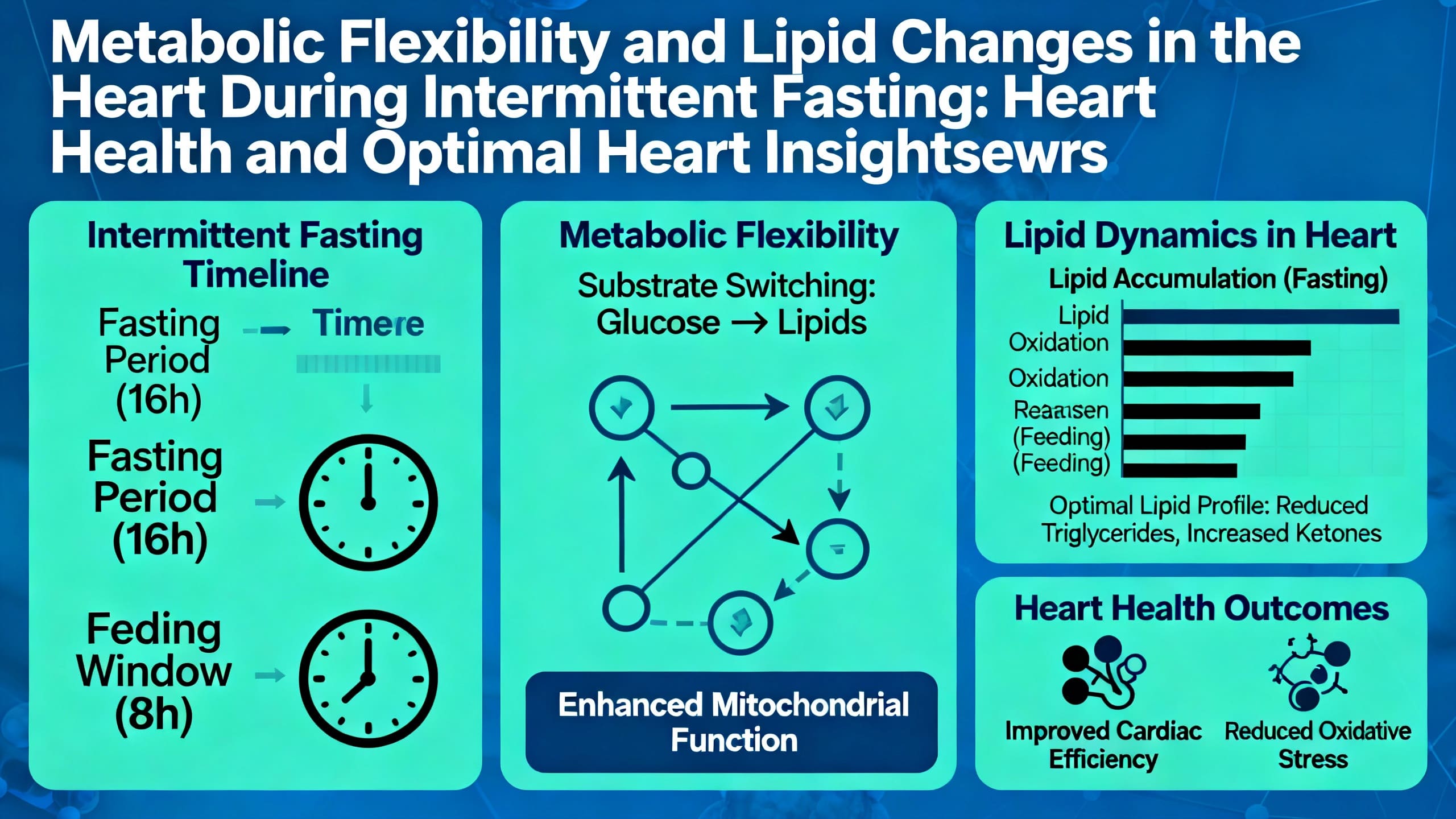
Time‑restricted eating refers to consuming all daily calories within a specific window, often 8–10 hours, and fasting for the remainder of the day. Alternate‑day fasting involves alternating between days of normal eating and days with significant caloric reduction or complete fasting. Metabolic flexibility is the body’s ability to switch efficiently between burning carbohydrates and fats for fuel—a process deeply tied to energy balance and cardiovascular health. These strategies originated from studies observing beneficial changes in metabolism and cellular health (de Cabo & Mattson, 2019; Patterson & Sears, 2017).
Benefits and Outcomes in Heart Disease
Evidence suggests that intermittent fasting methods can positively affect several cardiovascular risk factors:
- Reduced blood pressure: Both time‑restricted eating and alternate‑day fasting have demonstrated mild but significant reductions in blood pressure (Tinsley & La Bounty, 2015).
- Lower triglycerides and cholesterol: Improvements in lipid profiles—including lower triglyceride and LDL cholesterol levels—have been observed, contributing to optimal heart outcomes (Horne et al., 2020).
- Decreased inflammation: Fasting can suppress inflammatory markers associated with arterial plaque and atherosclerosis (de Cabo & Mattson, 2019).
- Enhanced insulin sensitivity: By promoting metabolic flexibility, intermittent fasting helps regulate insulin levels, further supporting heart health (Patterson & Sears, 2017).
Research Insights
Recent human clinical trials and systematic reviews have reinforced the link between intermittent fasting and improved cardiovascular outcomes:
- A 2022 systematic review found significant improvements in weight, body fat, and blood sugar control in those practicing time-restricted eating, all contributing to optimal heart health (Stockman et al., 2022).
- A randomized controlled trial noted that alternate-day fasting led to reductions in LDL cholesterol and markers of inflammation after 12 weeks (Templeman et al., 2020).
- Population studies have shown that intermittent fasting may decrease the risk of heart disease and related mortality, though more long-term studies are needed (Horne et al., 2020).
- Human and animal studies also indicate fasting can protect against cellular damage and improve arterial health (de Cabo & Mattson, 2019).
Practical Applications
Applying time-restricted eating or alternate-day fasting in daily life is increasingly feasible:
- Time-restricted eating (TRE): Common approaches include 16:8 (16 hours fasting, 8-hour eating window) or 14:10 patterns. Research supports 8–10 hour eating windows for most healthy adults (Patterson & Sears, 2017).
- Alternate-day fasting (ADF): Typically entails eating normally one day, and consuming 500–600 calories or no calories on the next. This approach may be challenging but shows benefits for overweight individuals (Templeman et al., 2020).
- Population suitability: These methods may not be suitable for pregnant individuals, those with a history of eating disorders, or people with certain metabolic conditions (Tinsley & La Bounty, 2015). Always consult with a healthcare provider, especially when heart disease risk is present.
Risks & Limitations
While the promise for heart health and an optimal heart is compelling, some risks must be considered:
- Short-term side effects: May include hunger, irritability, or headaches (Stockman et al., 2022).
- Research gaps: Most studies are short to medium term. Long-term effects on heart health and disease prevention require further observation (de Cabo & Mattson, 2019).
- Not for everyone: Medical supervision is necessary for those with pre-existing cardiovascular, metabolic, or eating disorders (Tinsley & La Bounty, 2015).
Key Takeaways
- Intermittent fasting, including time-restricted eating and alternate-day fasting, supports heart health and an optimal heart by improving blood pressure, cholesterol, and insulin sensitivity.
- Clinical studies show these techniques enhance metabolic flexibility, lower triglycerides, and help regulate inflammation.
- The best outcomes are seen when fasting regimens are paired with nutritious diets and are supervised, especially for those with existing heart health concerns.
- Risk of side effects is low for healthy adults, but some populations should avoid or closely monitor these strategies.
Frequently Asked Questions
1. Does time-restricted eating really improve heart health?
Yes, several human trials show that time-restricted eating can reduce blood pressure and improve cholesterol, supporting optimal heart outcomes (Stockman et al., 2022).
2. Is alternate-day fasting safe for those at risk of heart disease?
It can be, but requires medical supervision, especially in those with existing conditions, as fasting may interact with medications or blood sugar control (Tinsley & La Bounty, 2015).
3. Can intermittent fasting lower triglycerides and insulin?
Yes. Fasting protocols have been shown to reduce triglyceride levels and enhance insulin sensitivity (Horne et al., 2020).
Suggested Links
- American Heart Association – Heart-healthy diet and lifestyle
- National Institutes of Health – Time-restricted eating research
- PubMed – Intermittent fasting, heart disease, and metabolic health
Conclusion
Intermittent fasting, whether through time-restricted eating or alternate-day fasting, offers promising benefits for maintaining heart health and achieving an optimal heart. By favorably impacting blood pressure, lipid profiles, insulin levels, and inflammation, these dietary approaches can support both prevention and management of cardiovascular disease. However, it is important to tailor these strategies to individual health needs, consult healthcare professionals, and maintain a balanced diet to maximize heart health benefits. Start by exploring eating windows or fasting protocols that fit your lifestyle, but always prioritize safety and professional guidance for optimal heart outcomes.