Introduction
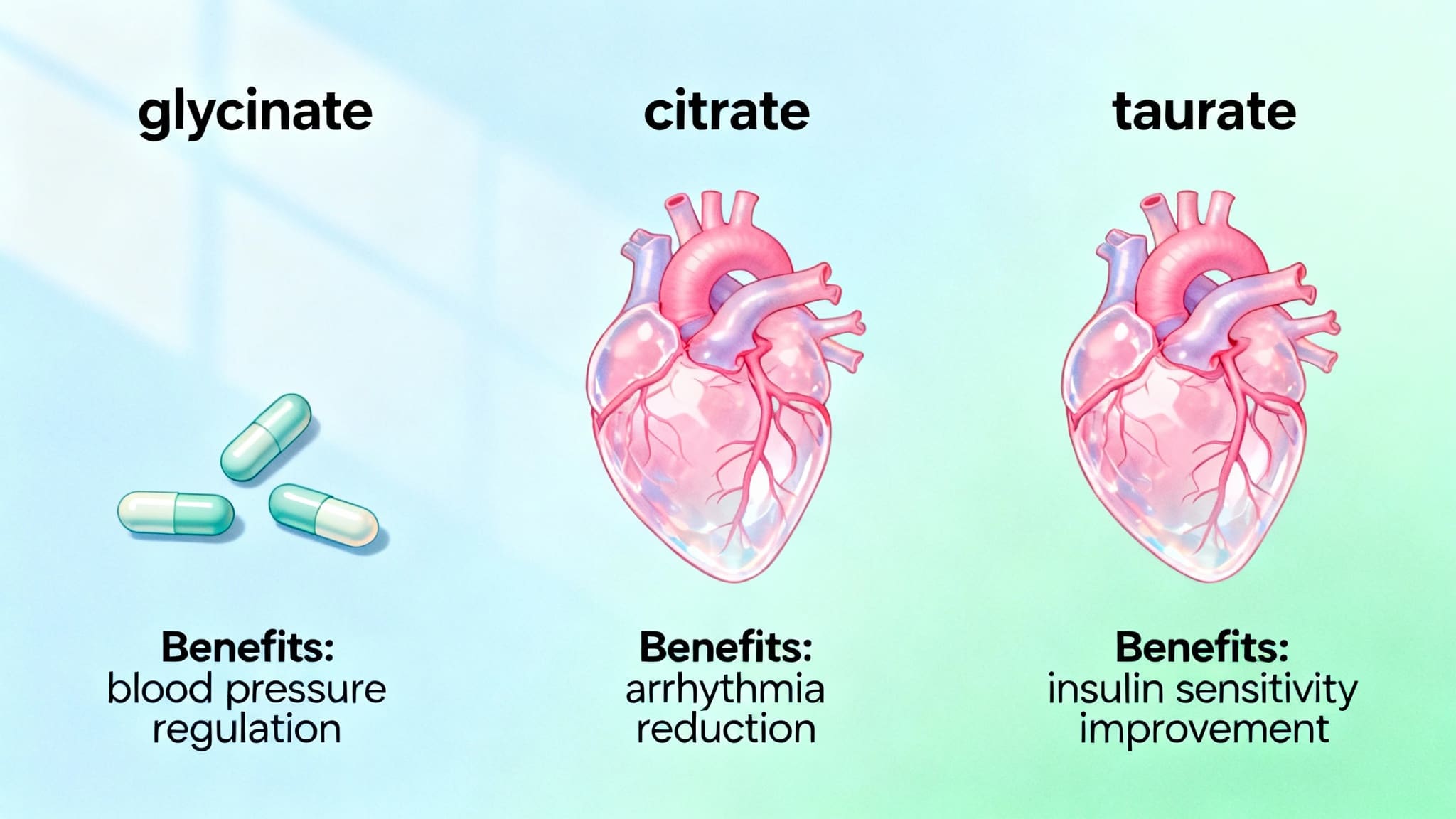
Magnesium is an essential mineral crucial to sustaining heart health and achieving optimal heart function. Research increasingly highlights the value of magnesium in regulating blood pressure, minimizing arrhythmia risk, and influencing insulin sensitivity—key factors for cardiovascular wellbeing. With multiple forms of magnesium supplements available—like glycinate, citrate, and taurate—knowing which fits specific heart needs is vital. This article explores magnesium’s wide-ranging impact on cardiovascular health, how different forms target various concerns, and how integrating the right type can support both prevention and treatment strategies for heart disease.
What is Magnesium’s Role in Blood Pressure, Arrhythmia Risk, Insulin Sensitivity, and Choosing the Right Form?
Magnesium is a mineral involved in over 300 biochemical reactions in the human body, many of which are fundamental for maintaining heart health. It helps blood vessels relax (vasodilation), supports normal rhythm in the heart, and plays a key role in glucose and insulin metabolism. Research recognizes its potential in lowering blood pressure and reducing irregular heartbeats (arrhythmias) (Rosanoff, Weaver & Rude, 2012). Historically, magnesium’s link to cardiovascular health was discovered when low intake correlated with higher rates of cardiovascular mortality (Song & Liu, 2012).
Benefits and Outcomes in Heart Disease
Regular magnesium intake is associated with improved blood pressure control and reduced arterial plaque buildup—significant contributors to heart health and the optimal heart. Studies show magnesium supplementation helps decrease systolic and diastolic blood pressure, supporting those at risk for hypertension (Zhang et al., 2016). Furthermore, magnesium plays a protective role against arrhythmias by improving electrical stability in heart muscle (Maksimovic et al., 2021). It also enhances insulin sensitivity, which lowers the risk of developing type 2 diabetes—a factor closely linked to heart disease incidence (Hruby & O’Donnell, 2022). Overall, magnesium’s anti-inflammatory and anticoagulant properties help maintain healthy arteries and minimize clotting risks, vital for optimal heart outcomes.

Research Insights
Recent studies emphasize the diverse benefits of magnesium for cardiovascular health. Human trials and meta-analyses reveal consistently that magnesium supplementation can modestly reduce blood pressure, especially in those with magnesium deficiency (Zhang et al., 2016). Randomized controlled trials have also demonstrated that magnesium supports electrical conductivity, thereby decreasing atrial and ventricular arrhythmias (Maksimovic et al., 2021). Systematic reviews further suggest that higher serum magnesium levels correlate with lower risks of insulin resistance and type 2 diabetes, critical for optimal heart health (Hruby & O’Donnell, 2022). Magnesium’s form matters: for example, magnesium glycinate and magnesium taurate are typically more gentle on the stomach and better absorbed, enhancing patient compliance (Schuchardt & Hahn, 2017).
Practical Applications
Incorporating magnesium into your daily regimen can be through diet or supplementation. Leafy greens, nuts, seeds, and whole grains are rich dietary sources. Supplementation is useful for those unable to meet needs via food alone.
-
Magnesium Glycinate: Best for those with sensitivities or sleep issues, given its calming effect. Typical dose: 200–400 mg/day (Schuchardt & Hahn, 2017).
-
Magnesium Taurate: Especially beneficial for heart rhythm regulation and blood pressure due to the addition of taurine, an amino acid with cardiovascular benefits (Zhang et al., 2016).
-
Magnesium Citrate: Highly bioavailable and often used for mild constipation relief; may suit those focused on magnesium repletion though less targeted for heart health than taurate or glycinate (Schuchardt & Hahn, 2017).
Populations who benefit most include adults with high blood pressure, arrhythmias, diabetes risk, or those on diuretics. Always consult a healthcare professional before starting supplementation.

Risks & Limitations
While generally well-tolerated, excess magnesium (usually from supplements, not food) can cause diarrhea, nausea, and, rarely, cardiac disturbances, especially in individuals with kidney disease (Rosanoff et al., 2012). Not all magnesium supplements are equally absorbed, and more research is needed to determine long-term outcomes in diverse populations. Some studies recommend caution in using high-dose magnesium in those with severe renal impairment. Quality of research varies, so clinical guidance and individualized assessment remain essential (Schuchardt & Hahn, 2017).
Key Takeaways
-
Magnesium is crucial for maintaining heart health and achieving an optimal heart, aiding blood pressure, rhythm, and glucose control.
-
The choice of magnesium form (glycinate, citrate, taurate) should match individual needs and tolerance.
-
Evidence links magnesium supplementation with reduced blood pressure, arrhythmia risk, and improved insulin sensitivity.
-
Dietary sources are preferable, but supplements can help at-risk populations.
-
Always consult a health professional for personalized advice and safe dosing.
Frequently Asked Questions
1. Which form of magnesium is best for arrhythmia and heart health?
Magnesium taurate is often highlighted due to its role in stabilizing heart rhythms, supported by recent clinical research (Maksimovic et al., 2021).
2. Can magnesium supplements help lower blood pressure?
Yes, studies show magnesium supplementation can modestly lower both systolic and diastolic blood pressure (Zhang et al., 2016).
3. Is magnesium safe for people with kidney issues?
People with severe kidney impairment should use caution and seek medical advice before taking magnesium, as improper clearance can lead to toxicity (Rosanoff et al., 2012).
4. Are dietary sources of magnesium enough to support optimal heart health?
For many, diets rich in nuts, leafy greens, and whole grains provide enough magnesium, but supplements may help those with deficiencies or higher cardiovascular risk (Hruby & O’Donnell, 2022).
Suggested Links
Conclusion
Magnesium is an underappreciated mineral that serves as a keystone for heart health and an optimal heart. By influencing blood pressure, rhythm, and metabolic factors, magnesium—whether from food or supplements like glycinate, taurate, or citrate—can be customized to individual needs for heart disease prevention and improved cardiovascular outcomes. Empowering yourself with the right information and working with your healthcare provider ensures you make the best decisions for an optimal heart. Start with a magnesium-rich diet or discuss supplementation as part of a holistic approach to cardiovascular wellness.