Introduction
Lipoprotein(a), often abbreviated as Lp(a), is a unique and genetically inherited cholesterol particle that plays a significant role in Heart Health. Despite its critical impact, many people are unaware of its connection to cardiovascular disease, making it an often overlooked factor in achieving an Optimal Heart. Recent advances in lipidology and genetic testing have highlighted the importance of measuring Lp(a), especially for those at increased risk of heart disease. If you are striving to understand all aspects of Heart Health and secure the best outcomes for an Optimal Heart, knowing your Lp(a) status is essential.
What is Lipoprotein(a)?
Lipoprotein(a) is a complex particle found in the blood, consisting of an LDL (“bad cholesterol”)-like core with an additional protein called apolipoprotein(a). Unlike traditional LDL cholesterol, Lp(a) levels are determined predominantly by genetics and are minimally influenced by diet or lifestyle. Elevated Lp(a) has been recognized as an independent risk factor for coronary heart disease, aortic stenosis, and stroke (Tsimikas & Hall, 2012).
Lp(a) was first identified in the 1960s and has since earned attention for its unique role in promoting atherosclerosis—the underlying cause of many heart attacks and strokes—making it a pivotal focus for advancing Heart Health (Emerging Risk Factors Collaboration, 2009).
Benefits and Outcomes in Heart Disease
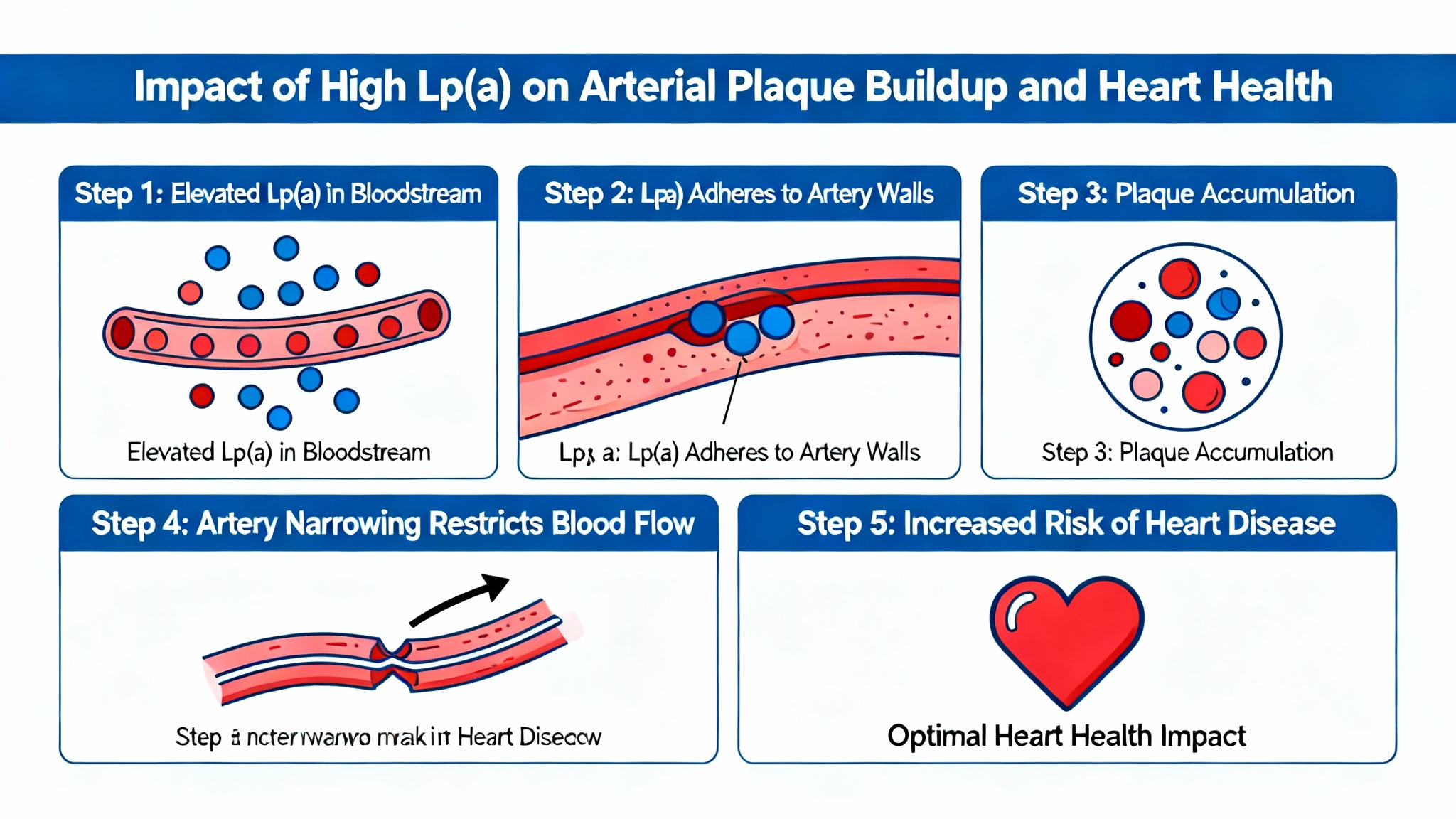
Addressing elevated Lp(a) levels can dramatically improve Heart Health and reduce the risk of arterial plaque buildup, heart attack, and stroke. High Lp(a) not only raises cholesterol but also worsens blood clotting and inflammation, making it a multifaceted risk factor. Studies have shown that individuals with Lp(a) in the highest quartile have a 2-4x increased risk of atherosclerotic cardiovascular disease compared to those with lower levels (Nordestgaard et al., 2010).
Novel therapies are being developed to specifically lower Lp(a), which is linked to improved cardiovascular outcomes and the potential for an Optimal Heart (Tsimikas et al., 2020).
Research Insights
Recent scientific research has categorized Lp(a) as one of the strongest inherited lipid risk factors for heart disease. Human studies have demonstrated that Lp(a) concentrations above 50 mg/dL are associated with a significantly higher risk of coronary events, even after accounting for traditional cholesterol levels (Emerging Risk Factors Collaboration, 2009). Interventional trials with novel RNA-based therapies—including antisense oligonucleotides—have reduced Lp(a) by up to 80%, showing promise in clinical endpoints (Tsimikas et al., 2020).
Current guidelines from the European Society of Cardiology and the American Heart Association recommend Lp(a) testing in individuals with premature cardiovascular disease or a family history of early heart disease (U.S. National Library of Medicine, 2022).
Practical Applications
Testing Lp(a) is a straightforward blood test and is especially important for anyone with a family or personal history of heart disease. Safe target ranges are generally below 30 mg/dL, with significantly increased risk seen above 50 mg/dL (Nordestgaard et al., 2010). While lifestyle changes may have limited impact—since Lp(a) is genetically set—a heart-healthy lifestyle, including not smoking, a Mediterranean diet, and exercise, is still vital for overall Heart Health and may help optimize other risk factors.
Therapies include PCSK9 inhibitors, lipoprotein apheresis, and emerging RNA-targeted medications. Individuals of African descent, those with premature heart disease, or those with unexplained high cholesterol should discuss Lp(a) testing with their healthcare provider (Tsimikas & Hall, 2012).
Risks & Limitations
While Lp(a) is a well-established risk factor, routine screening for everyone is not currently recommended due to varying prevalence and lack of universal access to testing. Additionally, most available cholesterol-lowering medications have minimal impact on Lp(a) levels. Some novel therapies are in late-stage clinical trials but are not yet widely available (Tsimikas et al., 2020). Potential side effects of apheresis and emerging drugs must be balanced against their cardiovascular benefits.
Key Takeaways
-
Lp(a) is a genetically inherited, potent risk factor for Heart Health—often missed in routine cholesterol checks.
-
Levels above 50 mg/dL significantly increase the risk for heart disease and reduce the chances for an Optimal Heart.
-
Only specific therapies and interventions can lower Lp(a), but testing helps personalize cardiovascular risk management.
-
Family history, early heart disease, or unexplained high cholesterol are key indications for Lp(a) testing.
-
Advances in therapies bring hope for more targeted treatment and improved Heart Health outcomes.
Frequently Asked Questions
1. Who should get their Lp(a) tested?
Anyone with a family history of premature heart disease, high cholesterol unexplained by lifestyle, or personal early heart events should consider Lp(a) testing (Nordestgaard et al., 2010).
2. Can diet and exercise lower Lp(a)?
Diet and exercise have little effect on Lp(a) since it’s genetically determined, but a heart-healthy lifestyle improves overall Heart Health (Tsimikas & Hall, 2012).
3. What treatments are available for high Lp(a)?
Current options include PCSK9 inhibitors and apheresis; RNA-targeted therapies show promise in lowering Lp(a) substantially (Tsimikas et al., 2020).
4. Are there any side effects to Lp(a)-lowering therapies?
Some therapies, such as apheresis and emerging drugs, can cause side effects and must be prescribed based on individual cardiovascular risk profiles (Tsimikas et al., 2020).
Suggested Links
Conclusion
Lipoprotein(a), or Lp(a), is a silent yet powerful player in the landscape of Heart Health and an Optimal Heart. Knowing your Lp(a) level could make a critical difference in accurately assessing cardiovascular risk and taking personalized steps for prevention and treatment. With new therapies approaching, now is the time to discuss Lp(a) testing with your healthcare provider and make proactive choices for lifelong Heart Health and an Optimal Heart.